Drug therapy
Drug therapy is the most important component of the treatment process. The success of the use of drugs is beyond doubt. Medicines have saved and are saving millions of lives and are an important achievement of our civilization.
The number of effective medicines is increasing every year. Modern drugs, on the one hand, can be extremely effective, and on the other hand, they carry the danger of severe side effects.
The age of the average patient is growing; the number of diseases he suffers from also increases. Consequently, the number of drugs shown to each patient increases. On the other hand, the use of a large number of drugs increases the risk of side effects, and possible interactions between them can affect the effectiveness. The doctor is faced with a difficult task: to build an optimal treatment regimen from a combination of the minimum of the most necessary drugs.
However, the most sophisticated drug regimen will not work if you do not follow the rules for its use. What matters is the time of taking the medicine, the frequency of taking, the relationship between taking the drug with food and compatibility with other drugs taken simultaneously.
It is important for the patient to have realistic goals of treatment, and the doctor needs to help him with this. Overestimation of drug therapy capabilities leads to disappointing results and reduced Compliance. Underestimation – to reduced patient motivation. Both options worsen treatment results.
Modern medicine is trying to replace the empirical approach in prescribing drug therapy to therapy based on an understanding of the factors that determine the response to treatment. However, each prescription of a drug carries elements of an experiment. Certain clinical effects are predicted, the possibility of side effects is taken into account, but the reaction to the drug always has its own individual characteristics. Therefore, in almost every case, the selection of a drug, combination, dose includes an element of empiricism, and the construction of an optimal therapeutic scheme takes time.
All medicines can be conditionally divided into two groups:
The first group consists of medicines, the effectiveness of which is assessed by changes in subjective and objective parameters. These are the patient’s well-being, blood pressure, blood sugar, pulse, weight, amount of urine excreted, etc. As a rule, the effects of drugs visible or felt by patients contribute to Compliance and there are no problems with taking drugs from this group.
The second group is drugs that improve the long-term prognosis for the patient.
As a rule, the purpose of their use is to prevent possible complications or slow down the progression of the disease. The healing effect of these drugs is difficult to quantify, and they can have side effects. It is very important for patients to understand this. Then they have no doubts about the need to take this drug for a long time.
The success of treatment depends on the successful interaction of both links of the doctor-patient axis.
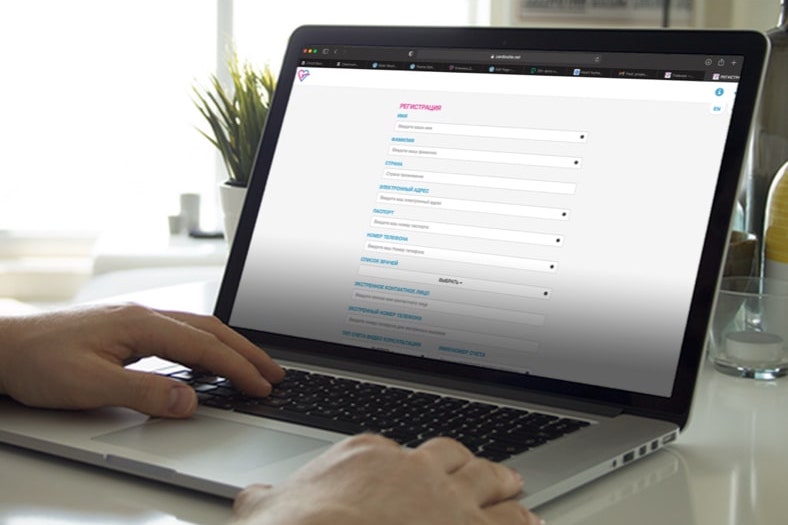
This requires: patient motivation, strict implementation of medical recommendations, awareness of the drugs used and understanding of the goals of their appointment. The implementation of the drug strategy requires strict adherence to the “technology”, that is, accurate implementation of the rules of application. Competent medication intake involves knowledge of the name and type of medication, the dose and frequency of its use, and the relationship between medication intake and food intake. The patient must know exactly what can happen and what to do if the medicine was not taken on time, how unexpected factors (stress, alcohol, bleeding …) can affect the effectiveness of treatment, what side effects are possible, and for what period the prescribed regimen is planned …
During treatment, sensitivity to the drug may change, and sometimes new side effects appear. Therefore, a monitoring mechanism is very important, which works according to the type of feedback and evaluates the indicators of the effectiveness of therapy specially selected by the doctor. The boundaries (symptoms or quantitative indicators) are determined, going beyond which requires immediate correction of treatment.
Over time, the patient himself learns the characteristics of his reactions to drugs, and this experience can be very useful for the doctor. Dynamic drug regimens can be used in the context of mutual trust between doctor and patient. They provide for changes in the dose or scheme by the patient himself within the framework established by the doctor.
The word pharmacology (the science that studies the effect of drugs on a person) comes from the Greek pharmakon, which translates as both medicine and poison. Indeed, along with the beneficial effects of any drug, there may be undesirable ones. Doctors are aware of many side effects associated with certain medications. Each appearance of new symptoms during drug treatment should be analyzed for possible side effects. It is also necessary to take into account the previous experience of taking drugs by patients and the development of side effects.
The spectrum of side effects is very wide: from minor, which can be neglected, to deadly, requiring immediate discontinuation of treatment and intensive therapy. Situations often arise when the doctor has to decide what is more important for the patient – the potential benefit of the treatment started or the harm of the developing side effects, and make a balanced decision.
The topic of drug negativism requires a special discussion. The feeling of psychological rejection is based on the vision of a drug as a harmful chemical that damages internal organs, evidence of the presence of a disease, a source of additional financial costs or a speculative product of pharmaceutical firms. This position is skillfully supported by “information specialists”, alternative medicine and Old Believer approaches, which in most cases do not provide an effective real alternative.
People who take the positions of drug negativism have a heightened sense of side effects, their expectation or a sense of fear of possible consequences. They may experience side effects even before the medication is used. Often there are suspicions of allergy to drugs that have not been used before. Initially not believing in the benefits of the medicine, “negativists” are in constant doubt and look for evidence of their innocence. Without following the doctor’s prescriptions, they see in themselves the competence to change the prescribed treatment and at the same time are surprised at the lack of effect.
Drug treatment options must be considered realistically and in a balanced way. Today, drug therapy is a part of our life, like other achievements of human evolution. If a person over the age of 50 does not take medication, this does not mean that he is healthy. Most likely, he did not go through modern medical screening, and his state of health is not a priority of his values. Conversely, drug prophylaxis in a person over 50 does not indicate the emerging illness.
The effect of a drug cannot be predicted by all or nothing categories.
A balanced drug strategy, justified by a professional doctor, comprehended and adopted by the patient, is able to really improve the course and prognosis of the disease in most cases.