Evidence based medicine
The term “evidence-based medicine” first appeared in the medical literature in the 90s of the twentieth century thanks to the work of G.P. Guyatt in epidemiology and statistics. Her idea is to use the most objective evidence-based arguments in the practice of medical decision-making. Evidence-based medicine emerged as an alternative to the empirical approach, which was based on the accumulated medical experience, generally accepted axioms and attached great importance to clinical thinking and medical intuition.
The rapid changes that took place in science and technology at the end of the 20th and beginning of the 21st century have closely affected medicine as a science. The information boom, often contradictory medical data, massive introduction of new drugs and technologies into the medical market, high dynamics of changes in approaches and concepts did not correspond to the existing empirical model.
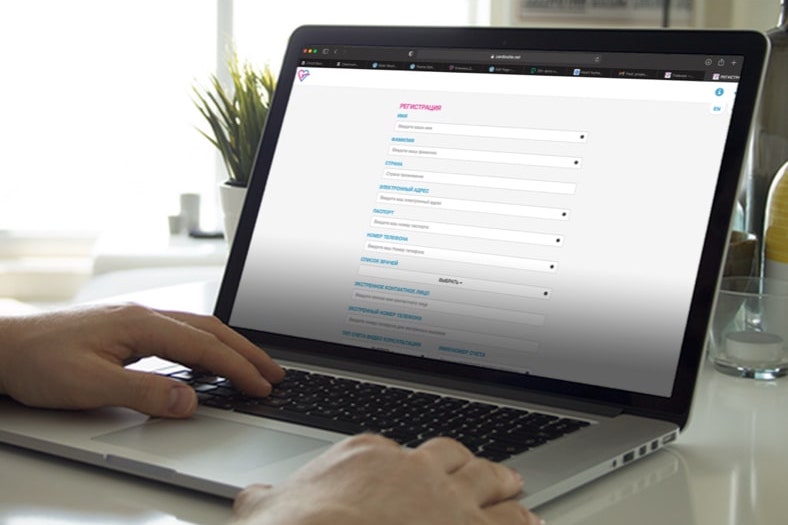
The result of globalization was the development of mutually related trends: standardization and centralization in medicine. The identification of approaches, the convergence and merger of medical schools, the migration of medical personnel, the international character of large pharmaceutical companies and corporations characterize the current trend. The computerization of health information has dramatically increased the importance and impact of health statistics. Now you can easily, quickly and efficiently analyze the needed facts and find a connection between them. The statistical standards of new level have become a necessary part of quality control in medicine. The requirements for conducting clinical trials have changed. This stage required compliance with the new concept. It was evidence-based medicine, medicine based on proven scientific facts.
Evidence-based medicine classifies the quality of evidence and distinguishes 3 levels of evidence for medical information. Level A – data obtained from a survey of large populations, many health centers, or several randomized trials. At the heart of the randomized trial is an objective comparison of homogeneous groups receiving one or another treatment alternative. A random distribution of objects (randomization) is performed before starting the study. The medical facts obtained in this way have proven clinical value. Level B – data obtained from a survey of relatively small populations by one large medical center (randomized), or the results of non-randomized clinical trials conducted by several medical centers. Level C – data obtained from a survey of limited population groups. The basis of medical knowledge is expert opinion and agreement, non-randomized clinical trials, generally accepted standards. The probative value of this level is the lowest.
The concept of evidence-based medicine is implemented at two levels: the creation of road map for treatment (guidelines), which are mandatory in medical practice, and the adoption of an individual medical decision (individual decision making), based on these principles.
The guidelines allow for the classification of indications for examination and treatment based on an assessment of the ratio of the potential benefit to the patient on the one hand, and the possible risk on the other. On the basis of this system, the patient’s clinical situation is classified into classes of indications. Class 1 – Procedure or treatment must be performed. The benefits of a procedure or treatment greatly outweigh the risk of potential complications. Class 2A – Performing a procedure or treatment appears reasonable. Benefit outweighs the risk of potential complications. Class 2B – The performance of the procedure or treatment should be discussed. Benefit slightly outweighs or equals the risk of possible complications. Class 3 – The risk of performing a procedure or treatment outweighs the potential benefit, meaning they should not be performed.
Each hospital or outpatient case is standardized for examination and treatment according to the established system of guidelines. Today this system is most developed in the USA and Europe. So in cardiology, the American ACC / AHA (www.heart.org) and European ECS (www.escardio.org) guidelines are widely used.
The principles of evidence-based medicine have greatly influenced modern medicine. Evidence-based medicine has changed the medical education system. Today, the emphasis in clinical medicine teaching is focusing on the study of guidelines, and students are assessed on their knowledge.
Evidence-based medicine is widely used in jurisprudence. The number of medical trials is on the upward trend. Medical errors and negligence are increasingly becoming the subject of legal proceedings. The principles of evidence-based medicine are a convenient basis for assessing the situation and making legal decisions.
Evidence-based medicine has unified the requirements for clinical trials. Conducted clinical trials must comply with its standards: GCP (good clinical practice), GMP (good manufacturing practice), GLP (good laboratory practice).
Evidence-based medicine has unified the requirements for the introduction of pharmacological and other medical products on the market. Its development is more in line with the missions of organizations responsible for protecting public health by ensuring safety, validation of the effectiveness of medicines, biological agents, devices and food products more than ever (for example, the government agency FDA in America).
Evidence-based medicine is good for many, but is it good for a particular patient? By definition, evidence-based medicine involves the use of scientifically proven facts in medical decision-making. But to what extent is the available evidence consistent with the individual clinical situation?
As an example, let us consider a randomized Partner trail, whose task was to compare the safety and efficacy of two treatments for a narrowed aortic valve: heart surgery and intravascular technique. The procedures were carried out in large clinics in the USA, Canada and Germany. After randomization (random distribution into groups of the same type of patients), the patients were divided into two groups. Patients of the first group were treated surgically, patients of the second group received treatment with intravascular technique.
Based on this examination, is it competent for a doctor to recommend the choice of a treatment method for a specific patient with a narrowed aortic valve in a clinic where the level of surgery is high and intravascular transplantation is low? Has this study answered the practical question – for which particular patient is surgery better (or worse), and for which is intravascular treatment better (or worse)? The Achilles’ heel of the concept of evidence-based medicine is the discrepancy between the method of scientific research, the object of which is an average abstract patient, and a personal medical decision for a specific medical situation.
The subject of evidence-based medicine study is a group suffering from a particular disease. An integrative approach – creating a model that includes the properties of its components, reflects the design of a scientific research. The model is the average patient, reflecting the properties of the studied group of patients as a whole. Any impact on the model (treatment, operation) and leading to a change in its properties characterizes the reaction of the studied group. Thus, the results of the study will reflect the impact on the group, characterize an abstract, average patient, reflecting the properties of this group. It is quite obvious that averaged conclusions cannot be automatically transferred to a real clinical situation. The biology and genetics of a particular patient, his concomitant diseases, socio-economic and psychological status, location and national characteristics, will distinguish him from the average, reflecting the properties of this group.
The main method of medical practice is clinical thinking. Clinical thinking is an analytical activity, thanks to which the doctor searches for medical symptoms, differentiating norm and pathology, distributes them according to their importance, integrates them into larger syndromes, differentiates diagnosis and medical concept, adapts knowledge, experience, recommendations of evidence-based medicine, intuition and crystallizes the medical solution into sick concept. The entire chain of medical thinking is based on analysis and differentiation, starting from diagnosis, understanding the patient, choosing a scientific basis for a concept, determining a medical solution. The qualifications and experience of the doctor, the real capabilities of a particular clinic, the level of the surgical or cardiological team – in the final stage, will determine what is best for the patient, and which treatment tactics are preferable.
Another serious problem in evidence-based medicine is the attempt to standardize the clinical manifestations of diseases. The clinical assessment of the patient’s condition is the cornerstone of medical practice. Diagnostics, situation analysis, functional assessment, medical decision, prognosis are impossible without an adequate clinical assessment of the patient. The patient’s clinical assessment contains a lot of subjectivity, ranging from the patient’s assessment of his own condition and feelings, to the doctor’s assessment of the patient’s condition, interpretation of his complaints, and research results.
For example, let us try to standardize such an important symptom in cardiology as shortness of breath during exercise in a patient with heart valve insufficiency. To the question – do you have shortness of breath during exertion? – patient A will answer no, although objective signs of shortness of breath will appear in him already after climbing the 2nd floor; patient B will answer – yes, although he will have shortness of breath only with a rapid ascent to the 7th floor; patient C will answer – yes, when climbing to the second floor, but his shortness of breath will primarily be associated with obesity, and not with valve insufficiency; patient D will answer I don’t know, because he suffers from leg problems and cannot walk. Clinical assessment of a patient is a medical art based on the experience, knowledge, personality and intuition of the doctor. The vision of the same patient by different doctors is different. The difference in clinical assessment can radically change the class of indications for examination and treatment in the same patient.
It is my personal experience that only one third of patients can be more or less objectively standardized based on the criteria of the guidelines. This weakness of evidence-based medicine is clearly understood by its advocates. While individual decision making based on evidence-based medicine is part of the concept, in real life, individualizing a medical decision tends to be a retreat from the recommended tactics in the guidelines.
Medicine is both a science and an art of healing. Acceptance of this fact means the need to combine in medical practice the achievements of science (today, basically, it is evidence-based medicine) and medical art (experience, vision, intuition, mission). The ability to make the right medical decision is the quintessence of medical practice. Only a truly competent physician can determine which is more dangerous: the risk of the procedure itself or refusal from it, and whether the procedure justifies the risk for a given patient. In what spatial dimension can all pros and cons be compared by constructing a total vector showing the correct choice?